Serious Incident Response Scheme
In residential aged care services in Australia, a Serious Incident Response Scheme (SIRS) will commence from 1 April, 2021. The SIRS will be administered by the Aged Care Quality and Safety Commission (the Commission) and will set new arrangements for providers of residential aged care to manage and take reasonable steps to prevent incidents, with a focus on the safety, health, well-being and quality of life of aged care consumers.
The SIRS includes both incident management and reportable incident obligations to strengthen aged care systems and build providers' skills so they are more able to respond to incidents and provide aged care recipients with the support they need
The SIRS includes both incident management and reportable incident obligations to strengthen aged care systems and build providers' skills so they are more able to respond to incidents and provide aged care recipients with the support they need
Why the SIRS is important
The Aged Care Quality and Safety Commission's website outlines the following reasons why the SIRS is important:
The SIRS requires every residential aged care service to adopt a systematic approach to minimising the risk of and responding to, serious incidents involving residents. The SIRS underscores the vital importance of an incident management system in helping every residential aged care service to effectively manage risks to their residents.
The SIRS also introduces explicit obligations for providers to report a broader range of serious incidents to the Aged Care Quality and Safety Commission (Commission) than is currently required under compulsory reporting obligations. This includes reports of all incidents that are alleged or suspected to have occurred, or witnessed, between consumers of an aged care service, including where the consumer who commits the incident has a cognitive or mental impairment (such as dementia).
Reportable incidents include ... Unlawful sexual contact or inappropriate sexual conduct – such as sexual threats or stalking, or sexual activities without consent.
Under the SIRS, an allegation, suspicion, or witness account of any of the above serious incidents must be reported to the Commission.
The SIRS requires every residential aged care service to adopt a systematic approach to minimising the risk of and responding to, serious incidents involving residents. The SIRS underscores the vital importance of an incident management system in helping every residential aged care service to effectively manage risks to their residents.
The SIRS also introduces explicit obligations for providers to report a broader range of serious incidents to the Aged Care Quality and Safety Commission (Commission) than is currently required under compulsory reporting obligations. This includes reports of all incidents that are alleged or suspected to have occurred, or witnessed, between consumers of an aged care service, including where the consumer who commits the incident has a cognitive or mental impairment (such as dementia).
Reportable incidents include ... Unlawful sexual contact or inappropriate sexual conduct – such as sexual threats or stalking, or sexual activities without consent.
Under the SIRS, an allegation, suspicion, or witness account of any of the above serious incidents must be reported to the Commission.
SIRS and sexual assault
KPMG was engaged by the Department of Health to conduct research into the prevalence of serious incidents in residential aged care. The Prevalence Study for a Serious Incident Report Scheme reviewed 178 residential aged care homes and identified an estimate of 1730 incidents of sexual assault nationally. It is worth noting that staff were asked to rate the impact of the incidents on residents and 58% said the sexual assault had no impact on the victim. Here are some key points from the KPMG report:
**
- The sample ratios can be combined with the national total estimates to provide an estimate of specific incident types. For example, the 4.4 per cent of incidents that were classified as being unlawful sexual contact can be combined with the total estimate of 38,898 incidents to provide an estimate at the national level of resident on resident incidents involving unlawful sexual contact (1,730 incidents). (page 5)
- A total of 56 Type 1** incidents were classified as unlawful sexual contact. The majority of the incidents that were reported as unlawful sexual contact displayed perpetrator behaviours of rape, sexual assault, including touching the resident’s genital area without consent (54.4 per cent). (page 33)
- Further analysis was undertaken on the 31 incidents that were categorised as displaying perpetrator behaviours of rape, sexual assault, including touching the resident’s genital area without consent. This further analysis looked at the victim impact for these incidents. The majority of these incidents (58.1 per cent) resulted in “no impact” on the victim. This result does appear somewhat anomalous. It might be expected that the perpetrator behaviour categorisation of “Rape, sexual assault etc.” may result a more “substantial” impact on the victim. Without further information on these particular incidents (e.g. through case notes) it is difficult to understand why these incidents were classified in this manner. (page 34)
- Eight options for the future reporting of resident on resident incidents in a SIRS were presented, and analysed. These include:
Option 1: Report all Type 1 and Type 2 incidents
Option 2.1: Report All Type 1 incidents only
Option 2.2: Report all Type 1 unreasonable use of force only
Option 2.3: Report Type 1 unlawful sexual contact only
Option 2.4: Report Type 1 incidents of a ‘higher’ level of impact only
Option 2.5: Report all Type 1 incidents triggering particular types of provider responses only
Option 2.6: Report all Type 1 unlawful sexual contact and all Type 1 unreasonable use of force associated with a higher level of impact only
Option 3: No change to the reporting requirements.
Each option was analysed, using the assessment principles of ease of application, level of reporting by services, regulatory response by the Commission, and the extent to which the option supported the capture of additional information on those incidents associated with the most harm. Based on this assessment, two preferred options were identified. These were Option 2.4 and Option 2.6. (page 6)
**
- Type 1 incidents: Resident on resident incidents that meet the Act’s definition of a reportable assault but which are exempt from being reported to the Department6
Type 2 incidents: Other resident on resident incidents which do not meet the definition of a reportable assault but are recorded by the approved provider.
Royal Commission's reflections on SIRS (February 2020)
The 2021 report on from the Aged Care Quality and Safety Commission included a number of reflections on the SIRS (see below from page 80):
- A serious incident reporting scheme is an important way to ensure that approved providers respond appropriately to incidents of abuse and neglect. The existing compulsory reporting scheme in aged care is unsatisfactory. It has a limited scope of incidents that must be reported, and information reported by approved providers is not used effectively.
- ... This [SIRS] scheme will require reporting of a much wider range of incidents than is currently the case. The expanded scope of incidents covered is a welcome development and will greatly improve the regulator’s oversight of abuse and neglect in residential aged care. However, expansion of the coverage of the scheme only addresses one of the defects in the current arrangements. Without an expansion of the scheme to home care, purposeful action on the reports of serious incidents, and greater transparency around the scheme, the abuse will continue.
- However, expansion of the coverage of the scheme only addresses one of the defects in the current arrangements. Without an expansion of the scheme to home care, purposeful action on the reports of serious incidents, and greater transparency around the scheme, the abuse will continue.
Guidelines for Residential Aged Care (March 2021)
In March 2021 the Aged Care Quality and Safety Commission launched Guidelines for Residential Aged Care Services that included the following information:
To assist providers with transitioning to the SIRS requirements reporting has been staged, from:
In May 2020 the Aged Care Quality and Safety Commission launched a series of fact sheets on reportable incidents, this includes a fact sheet on sexual assault. See link here or click on the image below.
To assist providers with transitioning to the SIRS requirements reporting has been staged, from:
- 1 April 2021 all ‘Priority 1’ incidents (incidents that have caused, or could reasonably have caused, a consumer physical or psychological injury or discomfort that requires medical or psychological treatment) within 24 hours.
- 1 October 2021 all ‘Priority 2’ incidents (all other reportable incidents that do not meet the criteria for a ‘Priority 1’) within 30 days.
In May 2020 the Aged Care Quality and Safety Commission launched a series of fact sheets on reportable incidents, this includes a fact sheet on sexual assault. See link here or click on the image below.
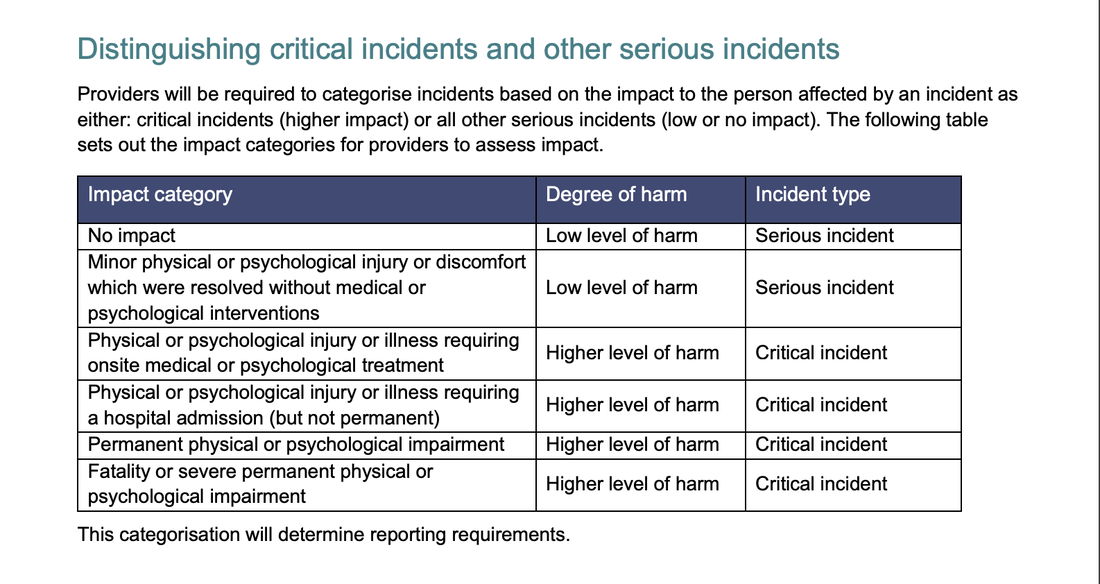
Distinguishing critical incidents and other serious incidents
A report on the Model for Operation of the Serious Incident Report Scheme identifies that staff will need to distinguish between critical incidents and other serious incidents (see page 13)
Providers will be required to categorise incidents based on the impact to the person affected by an incident as either: critical incidents (higher impact) or all other serious incidents (low or no impact). The following table sets out the impact categories for providers to assess impact.
Providers will be required to categorise incidents based on the impact to the person affected by an incident as either: critical incidents (higher impact) or all other serious incidents (low or no impact). The following table sets out the impact categories for providers to assess impact.
Priority 1 and 2 (pages 51-53)
The period of time within which to report a reportable incident to the Commission will depend on your categorisation of the incident based on your assessment as to the impact on the consumer. A reportable incident can be categorised as either as: a Priority 1 reportable incident, or a Priority 2 reportable incident.
A Priority 1 reportable incident includes any reportable incident that causes, or could have reasonably caused, a consumer physical or psychological injury or discomfort that requires medical or psychological treatment to resolve. In this instance, reportable incidents will be Priority 1 regardless of whether: the impact on the consumer is temporary or permanent; the medical or psychological treatment is provided at the service or elsewhere.
A Priority 1 reportable incident includes but is not limited to:
A Priority 2 reportable incident includes any reportable incident that results in a low level of harm to a consumer. In considering what is a low level of harm, consider the impact on the consumer.
Examples of low impact may include where the consumer is momentarily shaken or upset or where the consumer experiences temporary redness or marks that do not bruise. In these cases, where medical or psychological treatment for the consumer is not required, the reportable incident will be a Priority 2.
Where you are uncertain as to the impact, or where the impact appears low, but the consumer (or their representative) expresses ongoing distress or concern, the incident should be treated as a Priority 1.
If you have reasonable grounds to believe that a reportable incident is a Priority 1 reportable incident, the Commission must be notified within 24 hours of you becoming aware of the reportable incident.
Priority 2 reportable incidents must be notified to the Commission within 30 days of you becoming aware of the reportable incident.
A Priority 1 reportable incident includes any reportable incident that causes, or could have reasonably caused, a consumer physical or psychological injury or discomfort that requires medical or psychological treatment to resolve. In this instance, reportable incidents will be Priority 1 regardless of whether: the impact on the consumer is temporary or permanent; the medical or psychological treatment is provided at the service or elsewhere.
A Priority 1 reportable incident includes but is not limited to:
- consumer distress requiring emotional support or counselling
- cuts, abrasions, burns, fractures or other physical injury to a consumer requiring assessment and/ or treatment by a nurse, doctor or allied health professional
- bruising, including large individual bruises or a number of small bruises over the consumer
- head or brain injuries which might be indicated by concussion or loss of consciousness
- injury or impairment requiring the consumer’s attendance at or admission to a hospital
- the death of a consumer.
A Priority 2 reportable incident includes any reportable incident that results in a low level of harm to a consumer. In considering what is a low level of harm, consider the impact on the consumer.
Examples of low impact may include where the consumer is momentarily shaken or upset or where the consumer experiences temporary redness or marks that do not bruise. In these cases, where medical or psychological treatment for the consumer is not required, the reportable incident will be a Priority 2.
Where you are uncertain as to the impact, or where the impact appears low, but the consumer (or their representative) expresses ongoing distress or concern, the incident should be treated as a Priority 1.
If you have reasonable grounds to believe that a reportable incident is a Priority 1 reportable incident, the Commission must be notified within 24 hours of you becoming aware of the reportable incident.
Priority 2 reportable incidents must be notified to the Commission within 30 days of you becoming aware of the reportable incident.
Guidelines for Residential Aged Care - unlawful sexual contact
The above mentioned Guidelines include the following information on unlawful sexual contact (page 21-25):
Subsections 15NA(4) and (5) of the Quality of Care Principles expand on the meaning of unlawful sexual contact or inappropriate sexual conduct inflicted on the consumer to describe that unlawful sexual contact or inappropriate sexual conduct as including:
The Principles also provide that it is not a reportable incident where there is consensual contact or conduct of a sexual nature between the consumer and a person who is not a staff member, for example is another consumer at the service or a volunteer (other than while they are providing volunteer services). This ensures, for example, that a consumer who wishes to engage in a consensual sexual relationship with their partner, who is a volunteer at the service, is not prevented from doing so. In this scenario, it is expected that the provider would support both the consumer and the volunteer, such that volunteers working in an aged care service are clear as to what is appropriate conduct while engaged as a volunteer.
The definition also ensures that any conduct or contact of a sexual nature inflicted on the consumer by a staff member is always a reportable incident (i.e. consumer consent in this circumstance will not negate the requirement to report the incident).
While reports of unlawful sexual contact inflicted on a consumer were required under the previous compulsory reporting scheme, and providers will therefore be familiar with the concept, the requirement to notify incidents of this nature has been extended under the SIRS to also include inappropriate sexual conduct. This is consistent with similar incident reporting schemes, including the NDIS.
It is important to note that SIRS notification requirements are designed to protect vulnerable consumers, not to restrict their sexual freedoms. Unlawful sexual contact or inappropriate sexual conduct refers to non-consensual sexual activity involving consumers (unless the alleged offender is a staff member, in which case the incident must be notified).
Consumers’ right to maintain relationships of choice
Consumers have the right to have control over and to make choices about their personal and social life, including the right to sexual freedom and to give and receive affection. The Quality Standards require providers to support consumers to exercise choice and independence, including to make connections with others and maintain relationships of choice, including intimate relationships. It is expected that you will support the consumers at your service to maintain connections of importance to them. These rights and freedoms include consumers with a mental or cognitive impairment. This means you must balance your responsibilities in providing a safe environment for vulnerable consumers with the consumer’s right to maintain relationships of choice.
Understanding capacity to consent
Consent and decision making capacity are central to the requirements in the Quality Standards. You should therefore be familiar with assessing capacity and have existing systems and processes (including relationships with relevant health professionals who undertake such assessments) that support you to understand a consumer’s capacity to make informed decisions and provide consent. This may include speaking with a consumer’s family and/or carer to gain additional information and further understand the consumer’s capacity to consent, and ensuring that consumers are supported to effectively communicate their concerns, wishes and consent. It is acknowledged that consumers may have decision making capacity for some matters and not others and that capacity can fluctuate, including for consumers with cognitive impairment who may have moments of lucidity, such that their capacity to provide consent varies at different points in time. However, it is expected that your workforce is trained and equipped to manage issues of consent and determine a consumer’s ability to make decisions.
When considering the nature of a sexual contact, it can be useful for providers to consider the following questions:
Determining a consumer’s capacity to consent to sexual activity is a decision that may also be informed by an assessment by a health professional, which should be considered on a case by-case basis. If it is determined that the consumer has the capacity to consent to the particular activity at that particular time, and the consumer’s family and/or carer disagree with that assessment, providers should manage that through careful and sensitive discussion. Capacity to consent should be reviewed on a regular basis. If you have doubt about a consumer’s capacity to consent to an incidence of sexual contact, then the incident should be notified. Any incident of sexual contact that results in a consumer being distressed or upset should also be notified.
Important information for staff
At times staff may witness consumers engaging in activities that they are unsure about whether to report. For example, where they see a consumer kissing another consumer, or where a consumer has their hand under the clothing of another consumer. In determining whether the incident is reportable, staff should be encouraged to consider the person’s capacity to consent to the activity, and the relationship between the parties. It is critical to note that consumers with a cognitive impairment may not be aware or able to comprehend the nature of what is happening to them during sexual activity and in the absence of apparent resistance or obvious distress, staff may wrongly assume that “no observable impact” means the activity is consensual.
Broader commentary on unlawful sexual contact
There may be a range of emotional, behavioural, and physiological responses to unlawful sexual contact, including symptoms related to post-traumatic stress, such as depression and withdrawal. Sometimes these will mirror symptoms of cognitive impairment such as agitation, distress and confusion. There may be no discernible response. This does not mean that the person has not suffered from physical, emotional or psychological trauma.
What is not unlawful sexual contact or inappropriate sexual conduct?
What is unlawful sexual contact or inappropriate sexual conduct?
The above examples are illustrative only. Whether contact or conduct of a sexual nature is unlawful or inappropriate will need to be assessed in each individual case. For example, in the context of someone making a gesture of comfort, it is important to understand whether the consumer perceives that gesture to be comforting. Some consumers will be more comfortable with physical touch than others, and you will need to assess the situation based on your knowledge of the consumer and their relationships with those providing comfort.
Important information for staff
Staff are expected to engage with consumers appropriately and respectfully, and to maintain professional boundaries. For example, it is not appropriate to encourage consumers to engage with staff in a sexually inappropriate manner, such as telling sexual jokes or making sexual innuendos or crude comments.
Possible indicators of sexual assault (p. 43)
- if the contact or conduct is inflicted by a person who is a staff member of the provider or a person who provides care or services for the provider who is providing such care and services at the time of the incident (e.g. while volunteering):
- any conduct or contact of a sexual nature inflicted on the consumer, including but not limited to sexual assault, an act of indecency or sharing of an intimate image of the consumer
- any touching of the consumer’s genital area, anal area or breast in circumstances where this is not necessary to provide care or services to the consumer
- any non-consensual contact or conduct of a sexual nature, including but not limited to sexual assault, an act of indecency or sharing of an intimate image of the consumer
- engaging in conduct relating to the consumer with the intention of making it easier to procure the consumer to engage in sexual contact or conduct.
The Principles also provide that it is not a reportable incident where there is consensual contact or conduct of a sexual nature between the consumer and a person who is not a staff member, for example is another consumer at the service or a volunteer (other than while they are providing volunteer services). This ensures, for example, that a consumer who wishes to engage in a consensual sexual relationship with their partner, who is a volunteer at the service, is not prevented from doing so. In this scenario, it is expected that the provider would support both the consumer and the volunteer, such that volunteers working in an aged care service are clear as to what is appropriate conduct while engaged as a volunteer.
The definition also ensures that any conduct or contact of a sexual nature inflicted on the consumer by a staff member is always a reportable incident (i.e. consumer consent in this circumstance will not negate the requirement to report the incident).
While reports of unlawful sexual contact inflicted on a consumer were required under the previous compulsory reporting scheme, and providers will therefore be familiar with the concept, the requirement to notify incidents of this nature has been extended under the SIRS to also include inappropriate sexual conduct. This is consistent with similar incident reporting schemes, including the NDIS.
It is important to note that SIRS notification requirements are designed to protect vulnerable consumers, not to restrict their sexual freedoms. Unlawful sexual contact or inappropriate sexual conduct refers to non-consensual sexual activity involving consumers (unless the alleged offender is a staff member, in which case the incident must be notified).
Consumers’ right to maintain relationships of choice
Consumers have the right to have control over and to make choices about their personal and social life, including the right to sexual freedom and to give and receive affection. The Quality Standards require providers to support consumers to exercise choice and independence, including to make connections with others and maintain relationships of choice, including intimate relationships. It is expected that you will support the consumers at your service to maintain connections of importance to them. These rights and freedoms include consumers with a mental or cognitive impairment. This means you must balance your responsibilities in providing a safe environment for vulnerable consumers with the consumer’s right to maintain relationships of choice.
Understanding capacity to consent
Consent and decision making capacity are central to the requirements in the Quality Standards. You should therefore be familiar with assessing capacity and have existing systems and processes (including relationships with relevant health professionals who undertake such assessments) that support you to understand a consumer’s capacity to make informed decisions and provide consent. This may include speaking with a consumer’s family and/or carer to gain additional information and further understand the consumer’s capacity to consent, and ensuring that consumers are supported to effectively communicate their concerns, wishes and consent. It is acknowledged that consumers may have decision making capacity for some matters and not others and that capacity can fluctuate, including for consumers with cognitive impairment who may have moments of lucidity, such that their capacity to provide consent varies at different points in time. However, it is expected that your workforce is trained and equipped to manage issues of consent and determine a consumer’s ability to make decisions.
When considering the nature of a sexual contact, it can be useful for providers to consider the following questions:
- Does the consumer have the capacity to consent to this particular activity, at this time?
- Does the consumer have the capacity to refuse participation in the activity?
- Does the consumer have the capacity to agree to participate in the activity?
- Does the consumer show signs of distress?
Determining a consumer’s capacity to consent to sexual activity is a decision that may also be informed by an assessment by a health professional, which should be considered on a case by-case basis. If it is determined that the consumer has the capacity to consent to the particular activity at that particular time, and the consumer’s family and/or carer disagree with that assessment, providers should manage that through careful and sensitive discussion. Capacity to consent should be reviewed on a regular basis. If you have doubt about a consumer’s capacity to consent to an incidence of sexual contact, then the incident should be notified. Any incident of sexual contact that results in a consumer being distressed or upset should also be notified.
Important information for staff
At times staff may witness consumers engaging in activities that they are unsure about whether to report. For example, where they see a consumer kissing another consumer, or where a consumer has their hand under the clothing of another consumer. In determining whether the incident is reportable, staff should be encouraged to consider the person’s capacity to consent to the activity, and the relationship between the parties. It is critical to note that consumers with a cognitive impairment may not be aware or able to comprehend the nature of what is happening to them during sexual activity and in the absence of apparent resistance or obvious distress, staff may wrongly assume that “no observable impact” means the activity is consensual.
Broader commentary on unlawful sexual contact
There may be a range of emotional, behavioural, and physiological responses to unlawful sexual contact, including symptoms related to post-traumatic stress, such as depression and withdrawal. Sometimes these will mirror symptoms of cognitive impairment such as agitation, distress and confusion. There may be no discernible response. This does not mean that the person has not suffered from physical, emotional or psychological trauma.
What is not unlawful sexual contact or inappropriate sexual conduct?
- Consensual acts of affection such as greeting someone with a kiss on the cheek or a hug
- Consensual sexual relations between consumers, or between a consumer and their partner who is not a consumer at the service
- Gestures of comfort, for example a carer rubbing a consumer’s back or patting a consumer on the knee
- Helping a consumer to wash and dry themselves, where the carer is acting in accordance with applicable professional standards.
What is unlawful sexual contact or inappropriate sexual conduct?
- Any conduct or contact of a sexual nature inflicted on the consumer by a staff member or a person who provides care or services for the provider, while that person is providing such services (e.g. while volunteering)
- Sexual contact without the consumer’s consent, against their will or where consent is negated for other reasons such as lack of capacity to consent
- Having sexual intercourse or sexually penetrating a consumer (with a body part or an object) without consent
- Touching consumer’s genitals (or other private areas) without a care need
- A person masturbating, showing their genitals to a consumer or exposing themselves in the presence of a consumer
- Undressing in front of a consumer or watching consumers undress in circumstances where supervision is not required
- Inappropriate exposure of consumers to sexual behaviour of others
- Sexual innuendos, sexually explicit language or showing pornography to a consumer or using a consumer in pornography
- Grooming, stalking or making sexual threats to or in the presence of a consumer
- Forcing, threatening, coercing or tricking a consumer into sexual acts
- Unlawful sexual contact encompasses any behaviour of a sexual nature that is an offence under any criminal statute of a state, territory or the Commonwealth.
The above examples are illustrative only. Whether contact or conduct of a sexual nature is unlawful or inappropriate will need to be assessed in each individual case. For example, in the context of someone making a gesture of comfort, it is important to understand whether the consumer perceives that gesture to be comforting. Some consumers will be more comfortable with physical touch than others, and you will need to assess the situation based on your knowledge of the consumer and their relationships with those providing comfort.
Important information for staff
Staff are expected to engage with consumers appropriately and respectfully, and to maintain professional boundaries. For example, it is not appropriate to encourage consumers to engage with staff in a sexually inappropriate manner, such as telling sexual jokes or making sexual innuendos or crude comments.
Possible indicators of sexual assault (p. 43)
- Dropping hints that appear to be about abuse or making vague or incomplete references to unlawful sexual contact
- Sudden changes in behaviour or character, such as depression, anxiety attacks, or social or emotional withdrawal (e.g. crying, sweating, trembling, distress, agitation, anger, violence, absconding, seeking comfort and security)
- Bruises, pain, bleeding – including redness and swelling around breasts, thighs or genitals
- Presence of a urinary tract infection or unexplained sexually transmitted disease
- Torn or stained clothing or bedding • Avoiding or being fearful of a particular person (staff member, consumer or other)
- Sleep disturbances, refusing to go to bed, and/or going to bed fully clothed
- Refusing to shower
- Requesting a lock on their room.
Aged Care Legislation Amendment
In March 2021, the Aged Care Legislation Amendment (Serious Incident Response Scheme) Instrument was published. The amendment includes the following:
Unlawful sexual contact, or inappropriate sexual conduct
(4) In paragraph 54‑3(2)(b) of the Act, the expression “unlawful sexual contact, or inappropriate sexual conduct, inflicted on the residential care recipient” includes the following:
(5) However, that expression does not include consensual contact or conduct of a sexual nature between the residential care recipient and a person who is not a staff member of the approved provider, including the following: (a) another person who is a residential care recipient of the provider; (b) a person who provides care or services for the provider (such as while volunteering) other than while that person is providing that care or services.
Unlawful sexual contact, or inappropriate sexual conduct
(4) In paragraph 54‑3(2)(b) of the Act, the expression “unlawful sexual contact, or inappropriate sexual conduct, inflicted on the residential care recipient” includes the following:
- (a) if the contact or conduct is inflicted by a person who is a staff member of the approved provider or a person while the person is providing care or services for the provider (such as while volunteering)—the following: (i) any conduct or contact of a sexual nature inflicted on the residential care recipient, including (without limitation) sexual assault, an act of indecency and the sharing of an intimate image of the residential care recipient; (ii) any touching of the residential care recipient’s genital area, anal area or breast in circumstances where this is not necessary to provide care or services to the residential care recipient;
- (b) any non‑consensual contact or conduct of a sexual nature, including (without limitation) sexual assault, an act of indecency and the sharing of an intimate image of the residential care recipient;
- (c) engaging in conduct relating to the residential care recipient with the intention of making it easier to procure the residential care recipient to engage in sexual contact or conduct.
(5) However, that expression does not include consensual contact or conduct of a sexual nature between the residential care recipient and a person who is not a staff member of the approved provider, including the following: (a) another person who is a residential care recipient of the provider; (b) a person who provides care or services for the provider (such as while volunteering) other than while that person is providing that care or services.
Read more
- Serious Incident Response Scheme for Commonwealth-funded residential aged care – model for implementation
- Report on the Outcome of Public Consultation on the SIRS
- Prevalence Study for a Serious Incident Response Scheme, which looks at incidents of abuse between aged care residents
- Strengthening Protections for Older Australians: Development of Models and Options for a Serious Incident Response Scheme report